Six months ago Jo Tronc’s heart stopped on the operating table at Mackay Base Hospital.
Just moments after giving birth to a healthy baby girl some of the amniotic fluid that surrounded her baby entered her blood stream, triggering a catastrophic reaction.
Jo’s body plunged into cardiac and respiratory failure as her heart struggled to pump enough blood and the invading fluid caused life-threatening problems with blood clotting.
It took almost four minutes of CPR to restore her heart rhythm and the mum of two remained in an induced coma for two days in Intensive Care before her condition became more stable.
Fortunately the anaesthetic, surgical and obstetric teams at the Base instantly suspected the rare and often fatal amniotic fluid embolism (AFE).

Jo has little or no memory of the moment she almost died.
“Soon after she was born I said to my husband Mitchell ‘are you going to get some photos of her?’.
“He turned around to answer me and tells me I said ‘my chest’. My eyes rolled back and the alarms sounded. My heart had stopped,” Jo said.
“The staff had to quickly take him out of the theatre while they started CPR.”
Little Adaline was born on 5 October 2016 by caesarean section after Jo started having contractions and bleeding due to placenta praevia, a condition where the placenta is close to the cervix making a vaginal delivery too dangerous to risk.
“I had started bleeding and contracting and went to hospital around 10am. The obstetrician said we’ll do a caesarean now because it’s best to do them during the day when there’s a lot of staff around and by 1.30pm Adaline was born.”
Seconds after delivery fluid surrounding Adaline in the womb leaked into Jo’s blood stream, essentially causing an allergic reaction that sent her into cardiac and respiratory arrest.
The theatre team worked on her for nearly four minutes before establishing a cardiac rhythm again.
Doctors have told Jo she’s lucky to have survived and that most cases are generally diagnosed on autopsy.
Jo says the kindness of staff at the Base will be with her for ever and one name she recalls readily is anaesthetist Dr Lincoln Gan Lim, who knew she was anxious about the epidural and whether she would feel the birth.
“He was very good and made sure I was fully numb before they started cutting. He listened to my fears and took them seriously and made me feel better,” she said.
“From the moment I was in the waiting room for surgery he came over and made my husband fell like it was his day too – he made him feel comfortable as well as me. I was stressing out about feeling the caesar again like I did with my first baby. Lincoln actually said ‘we’re going to make this a good one for Jo’.
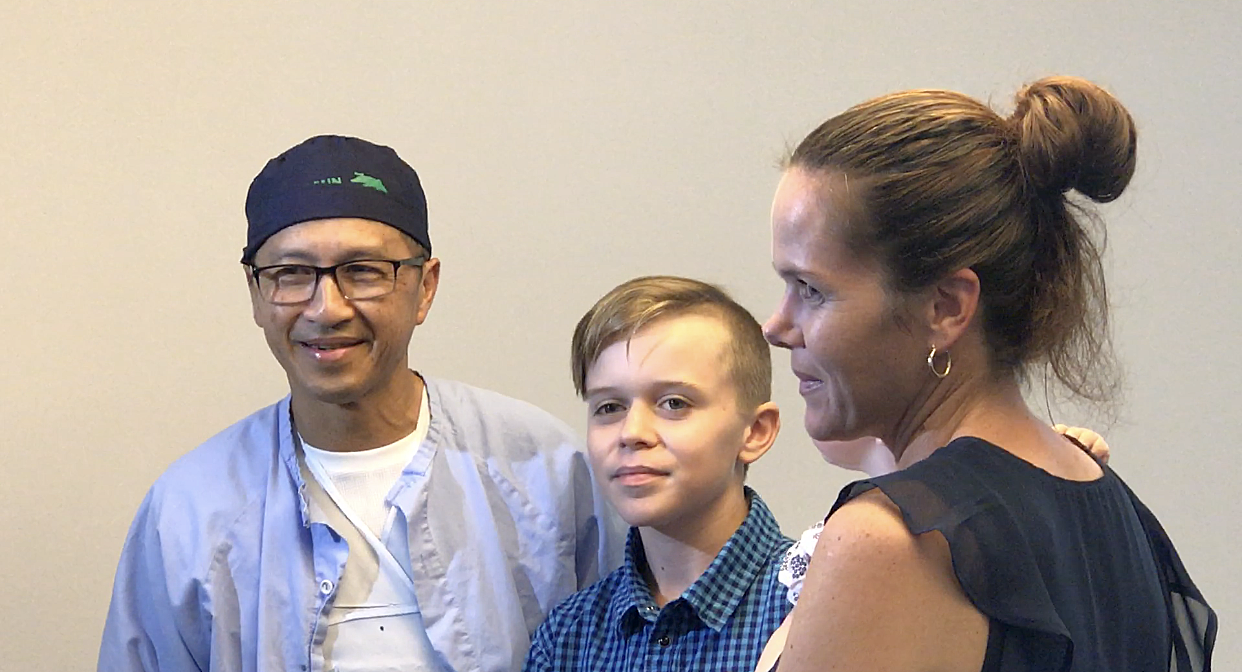
Anatesthetist Dr Lincoln Gan Lim
For Dr Gan Lim this story is more than him having a good bedside manner – it’s about the teamwork he says undoubtedly saved Jo’s life.
In his 30 years as an anaesthetist he has seen two women with an AFE and Jo is the only one to survive.
“Everything was fine, we were all OK, her husband was there, the baby came out and everyone was happy,” he recalled.
“It started as a pretty straight forward procedure, though we are always aware there might be some complications, and suddenly here you are. It’s the real thing happening.
“I knew I had to immediately intubate her, I said we have an emergency and I was just thinking we have to save her. I had a suspicion it might be an amniotic embolism as I’d seen one when I was a trainee doctor and had heard about one my colleague had at the old Base Hospital. I knew it has a high risk of death.
“There’s not time to think what is going on, no mucking around I just knew she needed an airway and that was my job.
Dr Gan Lim said Jo needed full CPR to be revived and she was moved to ICU.
“Jo is very lucky to be alive, she is one of the few good outcomes from AFE and I know a big reason for this is our team work and the fact our theatres and ICU are very well equipped.
“It’s very rare – we only have two to three minutes and if there had been a delay there could have been brain damage or death.
“There were many consultants, ICU was ready and waiting to accept her and it shows how good we are in a crisis,” Dr Gan Lim said.
A new machine lives up to its promise
ICU and pathology used the new ROTEM machine to determine exactly what blood products Jo needed.
She was among the first to benefit from the ROTEM (rotational thromboelastometry) just weeks after it was introduced just weeks earlier following a large amount of teamwork between theatre, ICU, pathology and emergency.
ROTEM reduce the use of precious blood products by 75% because it rapidly analyses bloods to decide what product in what quantity is needed to stop bleeding.
Mackay Base was the first regional Queensland hospital to have a ROTEM and it was announced with the promise it would save the lives of patients being treated after road crashes, birth complications or surgery.

Jo’s family and other supports
While AFE is something that “happened’ to Jo her whole family was impacted, not only by the trauma, but the events and care that followed.
“It was hard for Mitchell my husband, he saw it all, and had to leave the operating theatre while they were working on me. He actually saw them trying to save me and that is something he has struggled with.
“Everyone was great. Hannah, the midwife, was in theatre with me and also looked after me one night when I was on the ward. She was also wonderful with my family who flew in from Brisbane, the Gold Coast, Sunshine Coast and Airlie.
“The ICU girls were wonderful. When I woke up on the first things a nurse said to me was ‘Oh my god your son is amazing, he handle it like as trooper. The ICU staff kept him informed about what was happening and got him involved in look after me.
“He saw me the day after and he just crumbled and fainted. The nurses looked after him, got him some juice and explained everything to him.
“The whole family was well looked after by all of the staff, including social work. Little things like being flexible with visiting hours meant a lot.”
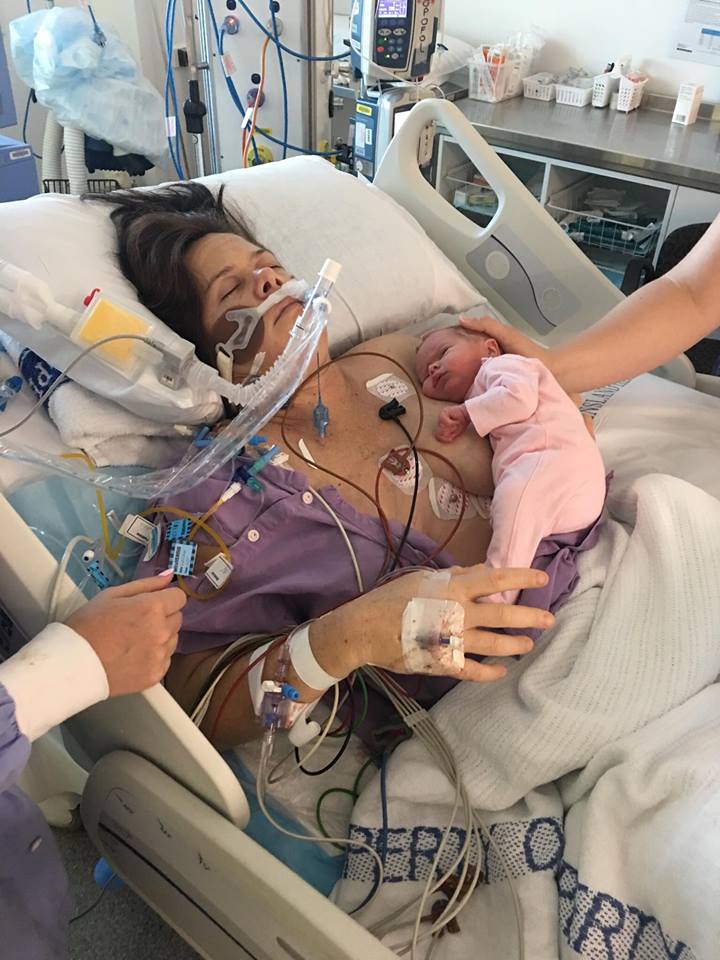
Jo had skin-to-skin contact with Adaline despite being kept in an induced coma.
“Adeline was fine, she went straight to Special Care Nursery because I couldn’t hold or feed her or do anything for her. My mum looked after her there.
“I came home on day seven – I was keen to get home. Mitchell had to give me daily injections and I was on strict bed rest. The midwives came to the house for a couple of months, there’s was good follow up care.
“My chest was incredibly sore from the CPR, it was three months before I could even clip a onesie together. It was a long recovery time.

Consultant Obstetrician Dr Ambreen Mansoor
The miracle of her survival hit home six weeks later when she sat down with Consultant Obstetrician Dr Ambreen Mansoor to talk through what had happened.
“She told me she had two previous patients with an amniotic fluid embolism, and that I was the first one she had been able to talk to. It was a very emotional conversation, we were both crying,” Jo said.
Speaking from Sydney where she now works, Dr Mansoor said AFE was a rare disorder with a high mortality rate and was impossible to predict.
“I heard the alarm and looked up to see Lincoln putting a tube in. They started the resus immediately and if it doesn’t happen in a timely way we can’t do much.
“We had just delivered the baby, they were doing CPR while we were closing.
“It was really fortunate Jo’s case happened with someone like Lincoln who was experienced to manage it. Because he had the tube in they could oxygenate her while we waited for heart to function again and circulate blood.
“The other thing in Jo’s favour it happened during the day time when there are more teams available to help.
“We were lucky to be there when literally everyone was available. It was an excellent team effort – there were so many hands there helping during and in the week that followed.
Jo went back to theatre later that night to stop a bleed, a complication from the body’s inability to clot and a bleeding vessel in the surgical field.
Her other equally important “patient” that still weighs on her mind is Jo’s husband.
“Jo was intubated and asleep and didn’t realise what was happening. But for her husband … I will never forget his face. He was the main person I was communicating with, to tell him what had happened, and that I had to take her back to theatre that night.
“We focus on the patient but the whole family that goes through the journey. His side of the story is very important
Dr Mansoor said it had been an amazing experience professionally and emotionally.
It was her second AFE since qualifying as an obstetrician 17 years ago.
“I have lost a close friend who was also an obstetrician to AFE so Jo’s story brought back a lot of memories for me of my friend,” Dr Mansoor said.
“I’m from Pakistan where I was trained and where I experienced my first AFE. Although the hospital was 10 times bigger than Mackay, the facilities were not as advanced.
“Now I am in Sydney and I can tell you a lot of bigger hospitals still don’t have the same facilities and equipment Mackay has.”
Staff Medical Officer in Obstetrics and Gynaecology Dr Ritu Rana
Dr Ritu Rana, who performed the caesarean section, had recently moved to Mackay from the UK where she worked in obs and gynae for 13 years.
“This was my first experience with AFE however obstetricians are prepared for it, we know about it, we do drills about it so we are prepared for this emergency but it is one of our worst nightmares,” Dr Rana said.
“I was operating on Jo doing the caesarean section and she we had just delivered the baby when suddenly she collapsed, and we heard the anaesthetist call the emergency buzzer and heard the thuds on her chest doing CPR and we knew straight away she had an AFE.
“We completed her surgery as soon as we could and were thinking ahead because the next thing after an AFE is a massive haemorrhage and we were preparing our trays ready for a hysterectomy.
“However her resus was so efficient she was revived in minutes and didn’t get to this stage. She made an amazing recovery thanks to the teamwork of everyone involved,” Dr Rana said.