It’s International Emergency Nurses Week and to help celebrate we’ll be giving a special insight into the Mackay Base Hospital Emergency Department.
Follow the below blog and experience the Emergency Department from the point of view of our nurses.
Friday, October 14
Merv | Security Officer
I work in the emergency response team which means I assist with responding to duress alarms or anything of that nature at the Mackay Base Hospital. Our office is based in the Emergency Department (ED) as it’s one of our busiest areas.
Unfortunately dealing with aggressive patients has become a regular occurrence for nurses in the ED and they see it in one form or another on a daily basis.
As they have to regularly face these situations, emergency nurses have been trained in de-escalation techniques to help calm down any aggressive patients. Many of them have also developed a thick skin and they take it in their stride. You can see the staff that are new to ED because they’ll be a little bit shocked or taken aback by how often they have to face these situations.
Patients need to understand that none of our staff want to see anybody wait for an extended period. Getting aggressive and angry won’t help the situation.
Emergency nurses and doctors are here to help and they understand that nobody wants to wait in ED if they are feeling unwell. Sometimes a patient who doesn’t appear as sick as another may require more urgent medical attention. The staff are extremely dedicated to giving all patients the best care and need to prioritise based on the level of care required.

Thursday, October 13
Robyn McCahill | Nurse Practitioner
I’ve been a nurse practitioner since 2009 and have been nursing for 33 years. I am normally stationed in Fast Track which sees patients that are unlikely to need admission to an inpatient ward. As a nurse practitioner it is my job to provide clinical care to patients presenting to ED. This is an autonomous role similar to that of a doctor as I see the patients, diagnose, investigate and treat the various complaints that present to the emergency department.
My twin sister, Sue, and I both work in the emergency department. We are now in different areas of the department however previously we both worked in fast track and it was fantastic. We communicate through non-verbal communication and she’ll already anticipate what I am about to do and I’ll anticipate her.
We get the double-take very often from both colleagues and patients. We’ve had a few times where colleagues insist they’ve told me information when really they’ve spoken to Sue. We’re identical, we sound the same and it’s near impossible to tell us apart and most people get a bit of a laugh out of it – we’ve had it our entire lives.
We think the same; send each other the same birthday and Christmas presents and even buy the same shoes!
What makes my sister a good nurse, or anyone a good nurse, is that they care. They care not just about themselves or their immediate patients but also about their colleagues. Working with your sister is like working with your best friend.

Wednesday, October 12
Mark Simpson | Registered Nurse
Nursing wasn’t my first career choice. After finishing school in Sarina I went to university to become a teacher but it wasn’t for me. I then worked as a sugar chemist at the mill and then went out to the mines testing coal and driving trucks as well as doing a lot of labouring work.
In 2008 I rolled my car and busted my arm. I was in the Base Hospital for a while and didn’t want to leave. It was such a change to be in a professional environment and watch the interaction between nurses, doctors and other professions.
I was down on my luck and feeling pretty bad. Dr San the orthopaedic doctor really cheered me up. I started to think then wouldn’t it be good to have a job where you could make people feel better physically and mentally. I thought about medicine but decided nursing was the better choice for me. I then went to CQU and did my degree.
I started working in mental health and moved to emergency nursing about 18 months ago. It’s a great career – there are so many ways you can advance your skills and work in different areas. It’s good to feel valued in a work place because of what you know.
I’m thinking about working in a rural hospital in the future so this is a great training ground. I really like my colleagues and my patients – you can’t be a nurse if you don’t like people!

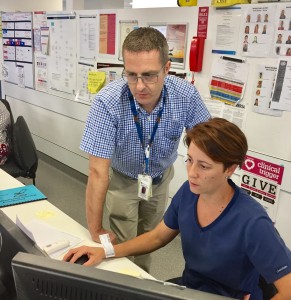
Dr Neale Thornton | Emergency Medicine Specialist
I tell this story to junior doctors to remind them to always listen to nurses. About six years ago back in the old ED an elderly man came in one night with chronic back pain. I was busy stitching up another patient and thought OK maybe he has a slipped disc and needs an x-ray, I’ll see him later.
Meanwhile one of the junior Registered Nurses noticed his condition was getting worse. He developed belly pain, sweating and his blood pressure dropped. She recognised he had a AAA – an abdominal aortic aneurism. This is basically when the major vessel that supplies bloody to the body ruptures and causes life-threatening bleeding.
The junior nurse told her senior who came and grabbed me and said you’ve got to come now, it’s an AAA. The patient was flown to Townsville by Flying Doctor and rushed into theatre around 3am and he made a good recovery.
This man got urgent care because the nurses were switched on. They did the right thing and he lived.
I tell the junior doctors that if a nurse comes and queries something you need to stop and check you are doing the right thing. It could well be that the nurse has thought of something you haven’t. Doctors and nurses are a team and we all come to work to do the best by our patients.
I still work with these two nurses Amber Daniel and Bec Goodworth – she’s the one in the picture with me today.

Tuesday, October 11
Elaine Joe | Resus
Today I’m allocated as resus nurse and am on standby for any seriously unwell patients who may come in. We have two Resuscitation Bays where the sickest patients are assessed and treated. So far this shift I’ve had one patient with chest pain with high risk cardiovascular disease. Fortunately he is doing well. In resus I start the patient assessment from the moment they arrive and at the same time I’m looking ahead pre-empting what may be required.
I try to build a rapport with my patients in a short period of time to gain their confidence. Keeping them informed about what we are doing and who the people are in the team looking after them is really important.
Another part of being a resus nurse is holding the Medical Emergency Team (MET) pager for any cardiac arrests in the hospital.
My background is acute care and emergency nursing. This is my fifth year with Queensland Health working in Emergency at Mackay. I rotate through different positions on each shift from acute bays, triage to Team leading.
I enjoy the variety and am passionate about working in acute care, hence why I still do this after many years.

Dr Peter Latham | Emergency Doctor
Emergency nurses are always hard working, extremely skilled and their experience is invaluable. They’re also fearless in getting things done and love the hustle and bustle of emergency.
Before going to med school in the UK I worked as a nursing assistant. This experience is something I believe all doctors should have to gain insight into nursing and the role a nurse plays. Working as a nursing assistant really helped me to realise I was on the right path.
The doctor and nurse relationship in emergency is very different. Due to the nature of our work we have the opportunity to work side-by-side with nurses in a very open environment. We all get busy in our roles and whenever anyone needs assistance there’s always someone to help no matter what their position.

Monday, October 10
Sue McGrath | High Dependency
I’m working in the High Dependency part of ED and my youngest patient is a 16 month old baby.
Rocco has come from Proserpine Hospital with his mum on the RACQ CQ Rescue helicopter after convulsing for a prolonged period.
He was stable when he arrived and the paediatric registrars have come very quickly to review him. After less than an hour in Emergency he’s off to the ward for further investigations into why he is unwell.
When we have patients arrive via chopper they are coming from rural areas needing access to health facilities quite urgently. In High Dependency we see most of these as they are the more acutely unwell patients triaged in at either a category two or three.
Once they are under my care I need to stabilise the patient by conducting a primary survey which includes A-B-C-D-E; Airways, Breathing, Circulation, Debility and Exposure. Once we’ve stabilised them and the doctor has put a plan in place, the patient then moves onto the ward for further care following a handover of information to the treating staff.
With so much variety working in the Emergency Department I can’t imagine myself anywhere else. I love working in this environment.

Carla Daly | Team Leader
My phone rarely stops ringing. The calls are varied – it can be the nurse manager wanting to know about patients who will need a bed or GPs letting me know about patients they are sending in. I also get calls about helicopter retrievals or patients transferring in from rural hospitals.
As team leader I allocate between staffing and patients, trying to match up the patients with the resources they need. For example if a patient deteriorates and becomes unwell they need to move to a different part of ED. I also need to make sure we have the right staffing and patient flow is managed so we are always prepared for anything that comes through.
It can be busy and you are continually reassessing your patients and what they need.
It’s challenging work, if you get to the end of the day and haven’t drowned you’ve done well. I like the job because it’s fast paced and we see a variety of patients.
My shift is nearly over now and I am prepping for hand over to the next shift.
Tori Harris | Triage Nurse
Working in the Emergency Department can be completely unpredictable as you never know who’s going to come through the doors.
As a triage nurse I do a rapid assessment on every patient that comes in and categorise them between numbers one, being the most critical, and five, who are less urgent.
Having to categorise all the patients means we do get very busy but that’s all part of the unpredictability of working as a triage nurse.
When there is a line of patients waiting to be triaged you just have to get in and work through as efficiently as possible. I’m also constantly looking ahead of the line to check there is nobody who may urgently need assistance.
Although it can be a challenging and busy environment we have a supportive team and none of us would be here if we didn’t want to help others.